At Veri, we often get asked, “Why should I monitor my blood glucose?”
It’s a great question — especially since glucose monitoring is often associated with having a health condition like diabetes. But monitoring blood glucose can be helpful for non-diabetics as well: it allows you to gain insights into your diet, nutrition, sleep, and hormones in a way that is personalized, frequent, and actionable.
Blood glucose: the big picture
Before we answer why you should monitor blood glucose, we need to understand the context. You may have heard that 88% of Americans are metabolically unhealthy, and public health data show that we have been on a downward trend as far as metabolic health goes for quite some time [1]. Cardiometabolic health has been declining for the past decade, and over 800 million people globally are living with obesity [2,3].
Poor metabolic health is also associated with a higher risk for chronic conditions like heart disease, diabetes, and obesity and is linked to inflammation, fatty liver disease, PCOS in women, and insulin resistance [4,5].
Why should non-diabetics monitor blood glucose?
1. The system is set up to treat people only after they’ve become pre-diabetic.
In its current state, the healthcare system only offers treatment for those who are pre-diabetic or diabetic.
You maybe see your doctor once a year and get routine bloodwork, but unless your levels of cholesterol, triglycerides, blood pressure, or fasting blood glucose meet the threshold of abnormality, it’s unlikely that you’ll know your metabolic health has changed in any way.
Clinical care is often better equipped to put out fires rather than prevent them — which leads to many of us continuing to have our metabolic health decline, all while thinking we are perfectly healthy.
2. Metabolic health is a spectrum.
Metabolic health is viewed as a binary: healthy or unhealthy.
But that’s not the way it works. Rather than black and white, metabolic health should be viewed on a spectrum, and there is a lot between being in peak health and developing Type 2 diabetes. Understanding where your health lies along this metabolic health spectrum is the first step toward protecting your health and preventing chronic conditions down the road.
3. People don’t know where they are on this spectrum.
Physical inactivity, poor nutrition (especially a diet high in processed foods), high levels of stress, and lack of sleep are all significant contributors to metabolic health declining over time. While we can become more active or try to eat better, the real issue is that metabolic health decline often happens without us knowing it.
Since symptoms of metabolic dysfunction tend only to show up when it becomes a severe issue, we’re often unaware of our metabolic health decline. Perhaps more importantly, people are unaware that there are tools to help them do something about it before their health reaches a point of concern.
4. You can’t predict metabolic unhealthiness by looking at someone.
It’s a common misconception that having an overweight or obese BMI indicates metabolically unhealthy. In the United States, it’s estimated that approximately 10% of adults are categorized as obese based on their BMI but are metabolically healthy, while 8% of adults are categorized as normal weight based on their BMI but are metabolically unhealthy [6].
5. Glucose variability and fluctuation matter as much, if not more than average glucose and fasting glucose.
Your blood glucose fluctuates throughout the day but is generally tightly regulated within a normal range by your body. However, when you repeatedly eat highly processed foods, skip exercise, miss sleep, and are stressed, your body’s ability to regulate your blood glucose effectively can begin to fall apart. This breakdown of effective glucose regulation is what slowly tips the scales toward metabolic dysfunction.
In both diabetic and non-diabetic people, research has shown that higher glucose variability is associated with the development of heart disease and oxidative stress, which can lead to chronic inflammation and is linked to obesity [7,8]. Similarly, glucose dips after a meal can predict hunger levels and the amount you eat, so achieving stable glucose levels may help curb cravings [9].
6. You can’t manage what you don’t measure.
We know that metabolic health is hard to predict, that we usually aren’t aware we’re metabolically unhealthy until we’re sick, and that glucose variability is an essential measure of health. So what can you do with this information? Monitoring your blood glucose is a great place to start. It gives you both immediate and long-term measurable data points that directly relate to your health.
Lifestyle interventions, like exercise programs and dietary changes, can be powerful tools for preventing chronic conditions [10]. One 30-year cohort study found that lifestyle interventions significantly reduced incidences of cardiovascular events and microvascular complications (like neuropathy, retinopathy, and nephropathy), reduced all-cause mortality from cardiovascular events, and increased life expectancy [11].
In other words, this stuff is preventable — and taking action by monitoring your glucose and adjusting your lifestyle accordingly before you reach a diagnosis may even help you live longer.
How can non-diabetics monitor glucose?
There are several ways to monitor blood glucose, but not all of them offer the same insights.
Hemoglobin A1C test
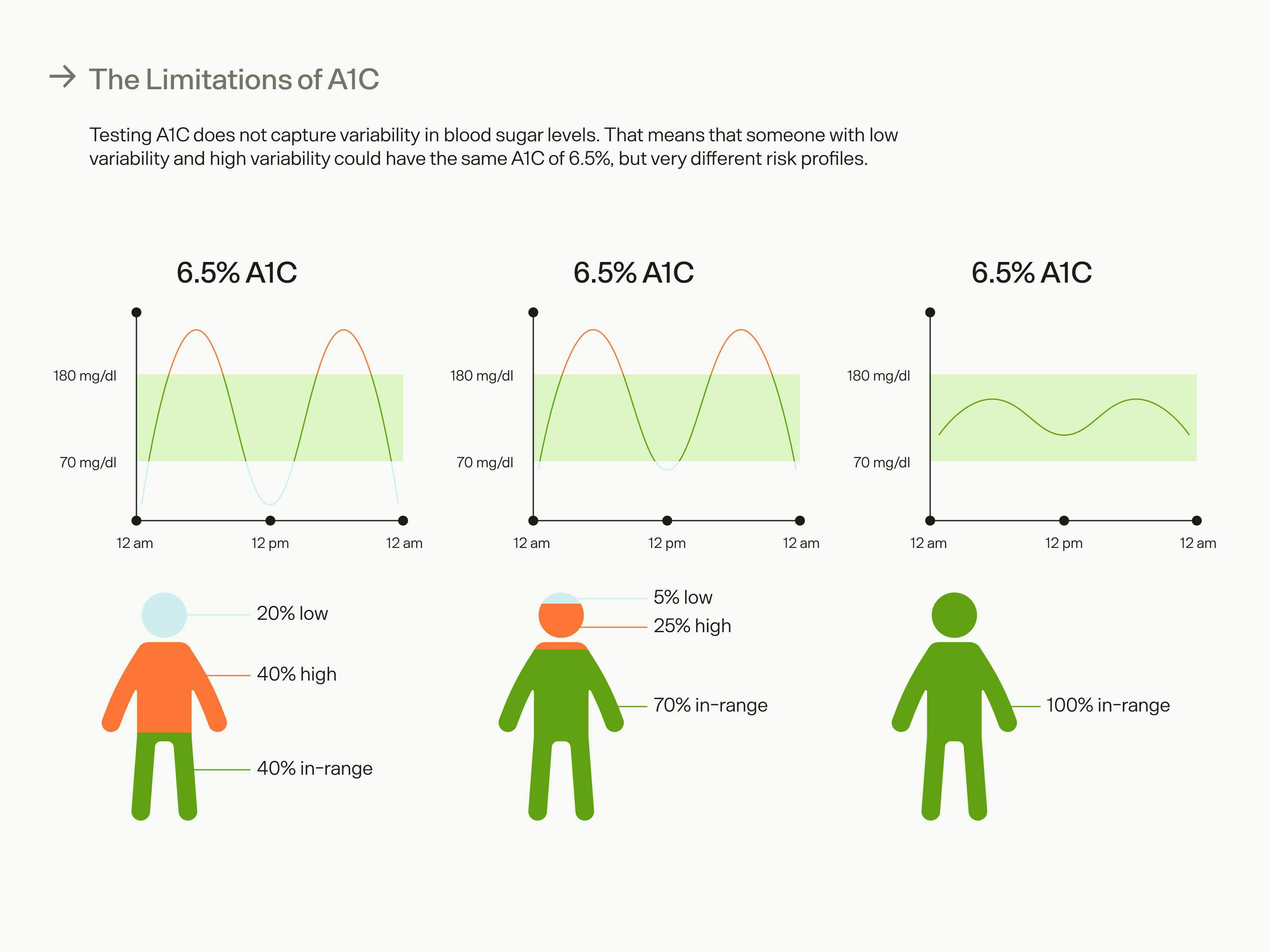
One testing method you may have heard of is the hemoglobin A1C test (hbA1C), which can be done at your doctor’s office via a blood draw. This test gives you an average blood glucose number for the past 3 months and is primarily used as a diagnostic tool for prediabetes and diabetes.
However, most people only get routine blood work once or twice a year, so you’re not getting the complete picture of what’s going on with your blood glucose levels, and if you notice any changes in your hbA1C, you won’t have comprehensive data to give you insights as to why these changes occurred.
Studies have shown that hbA1C is not as accurate in people who are nondiabetic when compared to diabetics, and hbA1C does not capture glucose variability, which we know is an important measurement for non-diabetics and diabetics alike [12].
Glucose tolerance test
A glucose tolerance test is another way to see how effective your body is at glucose uptake. This test is done at a doctor’s office and involves a blood draw followed by drinking a sugary beverage containing about 75g of sugar. After you drink this beverage, you’ll wait 2 hours, and have your blood glucose tested again. If your glucose is above 140mg/dL or 7.8 mmol/L, this indicates prediabetes or type 2 diabetes if it is above 200mg/dL or 13mmol/L.
Again, this is a diagnostic test that would be difficult to repeat at home constantly and does not offer any insight into the metabolic health spectrum, instead showing binary results.
Glucometer
Another option for monitoring glucose is using a glucometer to test your blood sugar, but this requires frequent finger pricks, which can be painful. It can also be challenging to interpret patterns, as the glucometer only shows you your blood glucose at that moment rather than over time.
CGM
A continuous glucose monitor, or CGM, is a small sensor you wear on your arm. It measures interstitial fluid to provide you with consistent glucose readings over the course of each day. A CGM, like the kind Veri uses, is painless to apply and lasts 14 days before it needs to be replaced. That’s 336 continuous hours of invaluable data about your body. You can see what your glucose levels are in real-time and your glucose response to food, exercise, and lifestyle factors. You’ll also see trends in your glucose fluctuations, fasting glucose, average glucose, and the time spent in the optimal range of 70 - 140 mg/dL, or 3.9 - 7.8 mmol/L.
What can a CGM show you that other methods can't?
Pairing a CGM with an app like Veri provides personalized insights on glucose trends and allows you to see the connection between your lifestyle and its effect on your health.
Since your glucose levels are affected by what you eat, physical activity, stress, sleep, and other lifestyle factors, seeing the glucose response show what habits may be hurting you and which interventions are working.
For example, you might want to test which “healthy” foods are serving your body and your goals. One reason prescriptive diets aren’t effective is that we all have a unique response to food, especially carbohydrates. A CGM can show you which ones to keep and which to kick.
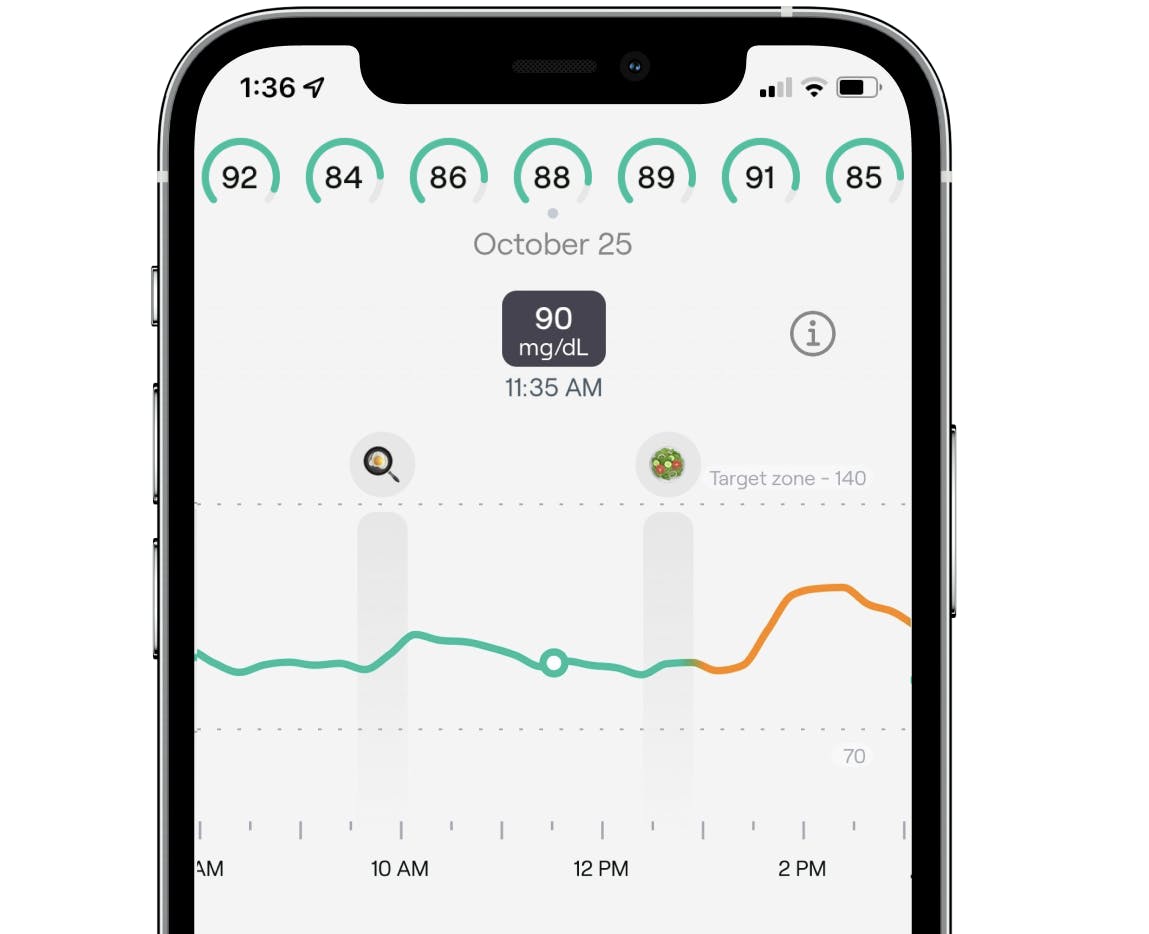
Continuous glucose levels in the Veri app, tracking your personalized glucose response to meals, workouts, and other life events.
Or, you might notice that the slump you feel every afternoon at work is due to elevated blood glucose levels, and you can experiment with changing your meal or trying after-lunch exercise to improve glucose levels and get your energy back.
If you discover that your glucose levels take over two hours to return to baseline after meals, you may be insulin resistant and can start incorporating things like strength training to increase your insulin sensitivity.
Perhaps most importantly, a CGM paired with an app like Veri gives you tools to become an active participant in your health long before any adverse health outcomes occur.
Prevention of chronic disease is much easier than managing one, and by understanding your blood glucose levels and the lifestyle factors that affect them, you can feel confident knowing you are actively protecting your health and well-being.
Can you get a CGM without a prescription?
In many countries, including the U.S., CGMs are considered medical devices and usually require a prescription from a healthcare provider. This applies whether you have diabetes or want to use a CGM for preventative reasons. If you’re a non-diabetic interested in glucose monitoring, you can skip a doctor’s visit and get a CGM prescription directly through Veri — you just need to fill out a questionnaire to confirm eligibility and upload your ID to verify identity.
Key takeaways
- Metabolic health is linked to myriad conditions, like heart disease, diabetes, obesity inflammation, fatty liver disease, PCOS in women, and insulin resistance. But with monitoring and lifestyle intervention, you can take steps to prevent chronic conditions.
- Metabolic health is a spectrum, and we often don’t know where we fall on this spectrum until we’re at the extreme and unhealthy end of it.
- Glucose variability and time in the range are helpful indicators of metabolic health that offer more insight than a one-time test.
- Glucose monitoring can show you where you are on the metabolic health spectrum and specifically what you need to change to improve your health.
- A CGM is the most effective and data-driven method of self-monitoring glucose both immediately and across time, helping you to detect trends and see your body’s real-time reaction to your health efforts.
Getting healthy doesn’t have to be confusing or complicated. Using your biological data to guide you, you can improve and protect your health in a way that works for you and your lifestyle.
References:
- https://www.liebertpub.com/doi/10.1089/met.2018.0105
- https://www.sciencedirect.com/science/article/abs/pii/S0735109722049944?dgcid=author
- https://www.thelancet.com/journals/landia/article/PIIS2213-8587(21)00058-9/fulltext
- https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.109.192644
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2780835/
- https://pubmed.ncbi.nlm.nih.gov/23970691/
- https://pubmed.ncbi.nlm.nih.gov/18299315/
- https://www.mdpi.com/1422-0067/12/5/3117
- https://academic.oup.com/cdn/article/4/Supplement_2/1611/5845141
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4360422/
- https://pubmed.ncbi.nlm.nih.gov/31036503/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2797987/